Abstract
Introduction and hypothesis
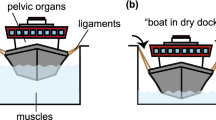
Pelvic organ prolapse (POP) affects one third of women of all ages and is a major concern for gynecological surgeons. In pelvic reconstructive surgery, native ligaments are widely used as a corrective support, while their biomechanical properties are unknown. We hypothesized differences in the strength of various pelvic ligaments and therefore, aimed to evaluate and compare their biomechanical properties.
Materials and methods
Samples from the left and right broad, round, and uterosacral ligaments from 13 fresh female cadavers without pelvic organ prolapse were collected. Uniaxial tension tests at a constant rate of deformation were performed and stress–strain curves were obtained.
Results
We observed a non-linear stress–strain relationship and a hyperelastic mechanical behavior of the tissues. The uterosacral ligaments were the most rigid whether at low or high deformation, while the round ligament was more rigid than the broad ligament.
Conclusion
Pelvic ligaments differ in their biomechanical properties and there is fairly good evidence that the uterosacral ligaments play an important role in the maintenance of pelvic support from a biomechanical point of view.

Similar content being viewed by others
References
Samuelsson E, Victor F, Tibblin G, Svardsudd K (1999) Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol 180:299–305
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark A (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Dietz HP (2008) The aetiology of prolapse. Int Urogynecol J 19:1323–1329
Alperin M, Debes K, Abramowitch S, Meyn L, Moalli PA (2008) LOXL1 deficiency negatively impacts the biomechanical properties of the mouse vagina and supportive tissues. Int Urogynecol J 19:977–986
Amundsen CL, Flynn BJ, Webster GD (2003) Anatomical correction of vaginal vault prolapse by uterosacral ligament fixation in women who also require a pubovaginal sling. J Urol 169:1770–1774
Buller JL, Thompson JR, Cundiff GW, Krueger Sullivan L, Schon Ybarra MA, Bent AE (2001) Uterosacral ligament: description of anatomic relationships to optimize surgical safety. Obstet Gynecol 97:873–879
Shull BL, Bachofen C, Coates KW, Kuehl TJ (2000) A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol 183(6):1365–1373
DeLancey JOL (1992) Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 166:1717–1724
Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B (2007) Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift technique)-a case series multicentric study. Int Urogynecol J 18:743–752
Conza NE, Rixen DJ, Plomp S (2007) Vibration testing of a fresh-frozen human pelvis: the role of pelvic ligaments. J Biomech 40:1599–1605
Cosson M, Boukerrou M, Lacaze S et al (2003) A study of pelvic ligament strength. Eur J Obstet Gynecol Reprod Biol 109:80–87
Reay Jones NH, Healy JC, King LJ, Saini S, Shousha S, Allen-Mersh TG (2003) Pelvic connective tissue resilience decreases with vaginal delivery, menopause and uterine prolapse. Br J Surg 90:466–472
Boukerrou M, Lambaudie E, Collinet P et al (2004) Mechanical resistance of pelvic ligaments used for incontinence or prolapse surgery. Gynecol Obstet Fertil 32:601–606
Vardy MD, Gardner TR, Cosman F et al (2005) The effects of hormone replacement on the biomechanical properties of the uterosacral and round ligaments in the monkey model. Am J Obstet Gynecol 192(5):1741–1751
Chen L, Ashton-Miller JA, Hsu Y, DeLancey JO (2006) Interaction among apical support, levator ani impairment, and anterior vaginal wall prolapse. Obstet Gynecol 108:324–332
Rubod C, Boukerrou M, Brieu M, Dubois P, Cosson M (2007) Biomechanical properties of vaginal tissue-Part 1: new experimental protocol. J Urol 178:320–5
Mooney M (1947) A theory of large elastic deformation. J Appl Phys 1940(11):582–592
Rivlin RS (1948) Large elastic deformations of isotropic materials. I. Fundamental concepts, II. Some uniqueness theorems for pure homogenous deformations. Philos Trans R Soc Lond Ser A:Math Phys Sci A240:459–490
Connell KA, Guess MK, Chen H, Andikyan V, Bercik R, Taylor HS (2008) HOXA11 is critical for development and maintenance of uterosacral ligaments and deficient in pelvic prolapse. J Clin Invest 118:1050–1055
Blaisdell FE (1917) The anatomy of sacro-uterine ligaments. Anat Record 12:1–42
Ramanah R, Parratte B, Hubert N, Arbez-Gindre F, Maillet R, Riethmuller D (2009) Anatomical and histological study of the uterosacral ligament: practical surgical consequences. J Gynecol Obstet Biol Reprod 38(4):304–311
Gabriel B, Denschlag D, Göbel H et al (2005) Uterosacral ligament in postmenopausal women with or without pelvic organ prolapse. Int Urogynecol J 16:475–479
Gabriel B, Watermann D, Hancke K et al (2006) Increased expression of matrix metalloproteinase 2 in uterosacral ligaments is associated with pelvicorgan prolapse. Int Urogynecol J 17:478–482
Goepel C (2008) Differential elastin and tenascin immunolabeling in the uterosacral ligaments in postmenopausal women with and without pelvic organ prolapse. Acta Histochem 110:204–209
Moalli PA (2005) Remodeling of vaginal connective tissue in patients with prolapse. Obstet Gynecol 106:953–963
Boreham MK, Miller RT, Schaffer JI, Word RA (2001) Smooth muscle myosin heavy chain and caldesmon expression in the anterior vaginal wall of women with and without pelvic organ prolapse. Am J Obstet Gynecol 185:944–952
Gabriel B, Rubod C, Brieu M, Dedet B, De Landsheere L, Cosson M (2011) Vagina, abdominal skin and aponeurosis: do they have similar biomechanical properties ? Int Urogynecol J 22:23–27
Martins P, Pena E, Calvo B, Doblaré M, Mascarenhas T, Natal Jorge R, Ferreira A (2010) Prediction of nonlinear elastic behaviour of vaginal tissue: experimental results and model formulation. Comp Meth Biomech Biomed Eng 13:327–337
Lei L, Song Y, Chen RQ (2007) Biomechanical properties of prolapsed vaginal tissue in pre- and postmenopausal women. Int Urogynecol J 18:603–607
Jean-Charles C, Rubod C, Boukerrou M, Brieu M, Dubois P, Cosson M (2010) Biomechanical properties of prolapsed or non prolapsed vaginal tissue: impact on genital prolapsed surgery. Int Urogynecol J 21:1535–1538
Acknowledgements
The authors announce unconditional financial support of the basic research by Ethicon Women’s Health & Urology. MS is a consultant of Ethicon Women’s Health & Urology. BG was awarded an International Fellowship grant by the International Urogynecological Association (IUGA) in 2009, which partly funded this research project. We thank Patrick Devos for his help with the statistical analyses.
Conflicts of interest
Géraldine Rivaux, Chrystèle Rubot, Bruno Dedet, Mathias Brieu declare that they have no conflict of interest to declare. Boris Gabriel: Serag-Wiessner (acceptance of paid travel expenses and honoraria). Michel Cosson: consultant for Ethicon and AMS, acceptance of paid travel expenses and honoraria, acceptance of payment for research; teaching sessions for Ethicon and Ipsen.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Rivaux, G., Rubod, C., Dedet, B. et al. Comparative analysis of pelvic ligaments: a biomechanics study. Int Urogynecol J 24, 135–139 (2013). https://doi.org/10.1007/s00192-012-1861-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1861-5