Abstract
Chronic severe facial pain is a feared sequel of cranial base surgery. This study explores the symptomatology, incidence and impact on the individual of postoperative de novo trigeminal nerve affection as well as the recovery potential. Out of 231 patients operated for cranial base meningiomas at the Karolinska University Hospital during 7 years, 25 complained of de novo trigeminal symptoms at clinical follow-up 3 months after surgery. Six were later lost to follow-up leaving 19 participants in the study, which was conducted using a questionnaire and a structured telephone interview. All patients complained of facial numbness, affecting the V1 branch in 10/19 patients (53%), the V2 branch in 18/19 (95%) and the V3 branch in 9/19 (47%). Surprisingly, only three (16%) suffered from trigeminal pain, which could be adequately managed by pharmacotherapy. However, five patients (26%) demonstrated ocular dysaesthetic problems. Twelve (63%) described their handicap to be mild, while seven (37%) had daily or severe symptoms. Five patients (26%) reported no improvement over time, while nine (47%) showed improvement and four (21%) stated good recovery. Only one patient (5%) claimed complete symptom remission. In the present study, 11% of the patients presented with a de novo postoperative affection of the trigeminal nerve after removal of a cranial base meningioma; 37% of these reported daily/severe symptoms. Only 26% showed good recovery, observed in patients without tumour infiltration of the nerve or intraoperative nerve damage. In spite of frequent complaints of numbness, pain was uncommon (16%) and often manageable by pharmacotherapy, while ocular symptoms turned out to be more frequent and more disabling than expected.

Similar content being viewed by others
References
Lang DA, Neil-Dwyer G, Garfield J (1999) Outcomes after complex neurosurgery: the caregiver’s burden forgotten. J Neurosurg 91:359–363
Mathiesen T, Gerlich Å, Kihlström L, Svensson M, Bagger-Sjöbäck D (2007) Hearing, facial and total outcomes in petroclival meningiomas operated with combined transpetrosal approaches. Neurosurgery 60:982–991
Dolenc VV, Kregar T, Ferluga M, Fettich M, Mozrina A (1987) Treatment of tumors invading the cavernous sinus. In: Dolenc VV (ed) The cavernous sinus: multidiciplinary approach to vascular and tumorous lesions. Springer, Wien, pp 377–391
Kawase T, Toya S, Shiobara R, Kimura C, Nakajima H (1987) Skull base approaches for meningiomas invading the cavernous sinus. In: Dolenc VV (ed) The cavernous sinus: multidiciplinary approach to vascular and tumorous lesions. Springer, Wien, pp 346–354
Sekhar LN, Sen CN, Jho HD, Janecka IP (1989) Surgical treatment of intracavernous neoplasms: a 4 year experience. Neurosurgery 24:18–30
Bender MB, Fulton JF (1944) Functional recovery in ocular muscles of a chimpanzee after section of oculomotor nerve. J Neurophysiol 1:144–151
Deruty R, Guyotat J, Mottolese C (1988) Recuperation partielle du nerf moteur oculaire commun après section puis reparation au cours de l’exerese d’une tumeur. Neurochirurgie 34:287–292
Fernandez E, Pallini R, Gangitano C (1987) Oculomotor nerve regeneration in rats. Functional, histological and neuroanatomical studies. J Neurosurg 67:428–437
Grimson BS, Ross MJ, Tyson G (1984) Return of function after intracranial suture of the trochlear nerve. Case report. J Neurosurg 61:191–192
Iwabuchi T, Suzuki M, Nakaoka T (1982) Oculomotor nerve anastomosis. Neurosurgery 10:490–491
Mark RF, Marotte LR (1972) The mechanism of selective reinnervetion of fish muscles. III. Functional electrophysiological and anatomical analysis of recovery from section of the IIIrd and 4th nerves. Brain Res 46:131–148
Nathan H, Goldhammer Y (1973) The rootlets of the troclear nerve. Anatomical observations in human brains. Acta Anat 84:590–596
Nathan H, Ouakine G, Kosary IZ (1974) The abducens nerve. Anatomical variations in its course. J Neurosurg 41:561–566
Saitoh K (1984) Oculomotor nerve anastomosis: an experimental study in the dog. No Shinkei Geka 12:1359–1366
Sandvoss G, Cervos-Navarro J, Yasargil MG (1986) Intracranial repair of the oculomotor nerve in cats. Neurochirugia 29:1–8
Sandvoss G, Stoltenburg-Didinger G, Yasargil MG (1987) Experimental transclival exposure and repair of the abducens nerve in cats. Neurochirurgia 30:65–68
Seifert V, Stolke D (1989) Laser-assisted reconstruction of the oculomotor nerve: an experimental study on the feasibility of cranial nerve repair. Neurosurgery 25:579–583
Sekhar LN, Lanzino G, Sen CN, Pomonis S (1992) Reconstruction of the third through sixth cranial nerves during cavernous sinus surgery. J Neurosurg 76:935–943
Keane JR, Baloh RW (1992) Posttraumatic cranial neuropathies. Neurol Clin 10:849–867
Stranjalis G, Sakas DE (2002) Post-traumatic transient bilateral trigeminal neuropathy. Acta Neurochir (Wien) 144:307–308, discussion 308
Yadav YR, Khosla VK (1991) Isolated 5th to 10th cranial nerve palsy in closed head trauma. Clin Neurol Neurosurg 93:61–63
Larson JJ, van Loveren HR, Balko MG, Tew JM Jr (1995) Evidence of meningioma infiltration into cranial nerves: clinical implications for cavernous sinus meningiomas. J Neurosurg 83:596–599
Sekhar LN, Möller AR (1996) Operative management of tumors involving the cavernous sinus. J Neurosurg 64:879–889
Sen C, Hagues K (1997) Meningiomas involving the cavernous sinus: histological factors affecting the degree of resection. J Neurosurg 87:535–543
DeMonte F, Smith HK, Al-Mefty O (1994) Outcome of aggressive removal of cavernous sinus menigiomas. J Neurosurg 81:245–251
Knosp E, Perneczky A, Koos WT, Fries G, Matula C (1996) Meningiomas of the space of the cavernous sinus. Neurosurgery 38:434–444
O’Sullivan MG, van Loveren HR, Tew JM Jr (1997) The surgical resectability of meningiomas of the cavernous sinus. Neurosurgery 40:238–347
Lopez de Armentia M, Cabanes C, Belmonte C (2000) Electrophysiological properties of identified trigeminal ganglion neurons innervating the cornea of the mouse. Neuroscience 101:1109–1115
Kohlhaas M (1998) Corneal sensation after cataract and refractive surgery. J Cataract Refract Surg 24:1399–1409
Lambiase A, Rama P, Bonini S, Caprioglio G, Aloe L (1998) Topical treatment with nerve growth factor for corneal neurotrophic ulcers. N Engl J Med 338:1174–1180
Chen HJ, Pires RT, Tseng SC (2000) Amniotic membrane transplantation for severe neurotrophic corneal ulcers. Br J Ophtalmol 84:826–833
Gybels JM, Sweet WH (1989) Neurosurgical treatment of persistent pain. Physiological and pathological mechanisms of human pain. Pain Headache 11:1–402
Meyerson BA, Hakanson S (1986) Suppression of pain in trigeminal neuropathy by electric stimulation of the gasserian ganglion. Neurosurgery 18:59–66
Holsheimer J (2001) Electrical stimulation of the trigeminal tract in chronic, intractable facial neuralgia. Arch Physiol Biochem 109:304–308
Linderoth B, Simpson B, Meyerson BA (2005) Spinal cord and brain stimulation (chapter 37). In: McMahon S, Kolzenburg M (eds) Wall and Melzack’s textbook of pain, 5th edn. Elsevier, Amsterdam, pp 563–582
Meyerson BA, Lindblom U, Linderoth B, Lind G, Herregodts P (1993) Motor cortex stimulation as treatment of trigeminal neuropathic pain. Acta Neurochir Suppl 58:150–153
Rainov NG, Heidecke V (2003) Motor cortex stimulation for neuropathic facial pain. Neurol Res 25:157–161
Morita A, Coffey RJ, Foote RL, Schiff D, Gorman D (1999) Risk of injury to cranial nerves after gamma knife radiosurgery for skull base meningiomas: experience in 88 patients. J Neurosurg 90:42–49
Leber KA, Bergloff J, Pedl G (1998) Dose–response tolerance of the visual pathways and cranial nerves of the cavernous sinus to stereotactic radiosurgery. J Neurosurg 88:43–50
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Ahmed Farhoud, Alexandria, Egypt
In the neurosurgical practice, sensory complications are usually underestimated by many treating physicians since they are based on a subjective complaint which could be assessed differently by different patients having the same complication.
In my opinion, this work covers a defective point in the literature, where complications related to the ocular motor nerves, facial nerve or lower cranial nerves palsies following skull base surgery are much more evident than complications related to trigeminal or olfactory nerve injury.
In this series, the authors present their experience with postoperative trigeminal neuropathy in a series of 231 patients treated for skull base meningioma. The study is based on subjective data given by patients with different tumour sites, from different age groups and with different pain thresholds. I personally think they could have used a standardized questionnaire (SF36 for instance) for better assessment. They can still cover this point in a future study.
Calculating the incidence of trigeminal complications among all patients operated for skull base meningioma is very deceiving as many of these tumours are not related to the trigeminal nerve. This is the case in most tuberculum sellae meningiomas and foramen magnum meningioma as an example. The study would have been more informative if the authors were more selective and chose meningiomas intimately related to the course of the trigeminal nerve as those involving the cavernous sinus and the petroclival region.
It is also important to outline the impact of surgical approach on such complications. Diminished lacrimation does not necessarily mean V1 injury; it could be the result of greater superficial petrosal nerve injury during drilling of the petrous apex. It is not clear in this paper if some of the sensory complications mentioned are related to the approach rather than the original pathology as in supraorbital nerve injury for instance.
However, this work presents the experience of the authors with postoperative trigeminal neuropathy in a clear and descriptive way. It sends an important message that some of the operative complications seen as “minor” by treating physicians could affect the patients’ quality of life significantly.
Andreas K. Demetriades, London, UK
Patient-reported outcomes and QALYs are increasingly recognised as a tool for outcome measures and therefore as an influential parameter in deciding between available treatment options. The neurosurgical department at the Karolinska has previously shown how trigeminal neuropathy has a large influence on postoperative health status perception by the patient [22]. This study builds on the previous by documenting the postoperative complications affecting the trigeminal nerve in patients undergoing surgery for skull base meningiomas, in whom there were no preoperative trigeminal nerve complaints.
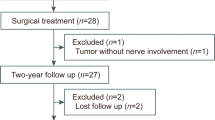
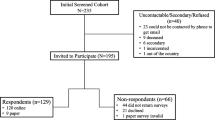
Over a period of 7 years (1997–2003), 25 out of 231 patients (11%) with skull base meningiomas complained of de novo postoperative trigeminal nerve symptoms at 3 months. Six were lost to subsequent follow-up. Of those studied (n = 19),- all (19/19) had facial numbness (V2 > V1 > V3).- 5/19 had an impaired corneal reflex/corneal ulceration/ocular symptoms, either due to V1 injury or greater superficial petrosal nerve-related injury (dry eye).- 3/19 had facial pain (V2 > V1).- 2/19 had trigeminal motor loss.
The authors analysed the grade of severity for these symptoms, which seemed worse when there was cavernous sinus invasion, and the degree of recovery. The majority (10/19) showed little or no recovery, and only 2/19 showed good recovery or resolution of symptoms.
As the authors point out, limitations of this study need to be considered:- This is a retrospective study with potential recall bias.- Tumour location was heterogeneous. It is clear from the data that the highest incidence of postoperative trigeminal neuropathy was in the group with cavernous sinus involvement (≈60%). There was little further analysis as to the impact of location, which included meningiomas in the anterior, middle and posterior cranial fossae. Indeed, due to the small sample size, this would have been difficult.- Information and potential correlation between the amount of tumour resection (or residual) and symptom severity in different tumour locations would have been interesting.- The study population excluded patients with trigeminal symptoms preoperatively, and the reasons have been well explained. This would be a useful comparison, however, which will allow an assessment of the susceptibility of the trigeminal nerve with respect to different tumour locations and/or different operative approaches.
Overall, this is a very interesting and useful contribution to the skull base meningioma literature and should provide a good basis for prospective studies and analyses between tumour location, operative strategy, trigeminal neuropathy and risk stratification. This would help construct a framework for doctors and patients regarding treatment choices and complication avoidance.
Nicholas C. Bambakidis, Cleveland, Ohio, USA
The article by Westerlund et al. provides a review of a large series of cranial base meningiomas and a well-known but rare complication of such surgery, namely trigeminal complications. Important results of the current study include the results of some degree of trigeminal symptoms in 11% of patients. All patients complained of facial numbness, most commonly in the V2 branch (95%). Symptoms of pain were rare (16%), and all symptoms were resistant to improvement over time with only 21% stating a good recovery and only one patient claiming complete remission. Interestingly, patients with preoperative trigeminal symptoms were excluded. It would be interesting to gauge the response to surgical treatment in this population of patients regarding whether their symptoms improved or worsened since in my anecdotal experience, their symptoms improved after surgery. In any event, the results are important in including the risk of such complications when preoperative counselling of patients is performed.
Rights and permissions
About this article
Cite this article
Westerlund, U., Linderoth, B. & Mathiesen, T. Trigeminal complications arising after surgery of cranial base meningiomas. Neurosurg Rev 35, 203–210 (2012). https://doi.org/10.1007/s10143-011-0355-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-011-0355-0