Opinion statement
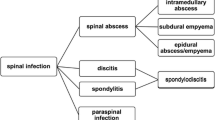
Subdural empyema represents loculated infection between the outermost layer of the meninges, the dura, and the arachnoid. The empyema may develop intracranially or in the spinal canal. Intracranial subdural empyema is most frequently a complication of sinusitis or, less frequently, otitis or neurosurgical procedures. Spinal subdural empyema is rare and may result from hematogenous infection or spread of infection from osteomyelitis. The most common organisms in intracranial subdural empyema are anaerobic and microaerophilic streptococci, in particular those of the Streptococcus milleri group (S. milleri and Streptococcus anginosus). Staphylococcus aureus is present in a minority of cases, and multiple additional organisms, including Gramnegative organisms, such as Escherichia coli, and anaerobic organisms, such as Bacteroides, may be present. Pseudomonas aeruginosa or Staphylococcus epidermidis may be present in cases related to neurosurgical procedures, and Salmonella species have been detected in patients with advanced AIDS; multiple organisms may be present simultaneously. Spinal subdural empyemas are almost invariably caused by streptococci or by S. aureus. Subdural empyema—whether it occurs in the skull or the spinal canal—may cause rapid compression of the brain or spinal cord, and represents an extreme medical and neurosurgical emergency. The diagnostic procedure of choice for intracranial and spinal subdural empyema is MRI with gadolinium enhancement. Computed tomography scan may miss intracranial subdural empyemas detectable by MRI. Conversely, occasion spinal subdural empyemas may be detected by CT myelography where MRI is negative. Treatment in virtually all cases of intracranial or spinal subdural empyema requires prompt surgical drainage and antibiotic therapy. Pus from the empyema should always be sent for anaerobic, as well as aerobic, culture. Because intracranial subdural empyemas may contain multiple organisms, provisional antibiotic therapy of intracranial subdural empyema, where the organism is unknown, should be directed against S. aureus, microaerophilic and anaerobic streptococci, and Gram-negative organisms. Antibiotics should include 1) nafcillin, oxacillin, or vancomycin; plus 2) a third generation cephalosporin; plus 3) metronidazole. Provisional antibiotic therapy of spinal subdural empyemas should be directed against S. aureus and streptococci, and should include nafcillin, oxacillin, or vancomycin. Morbidity and mortality in intracranial and spinal subdural empyema relate directly to the delay in institution of therapy. Both conditions should, thus, be treated with great urgency.
Similar content being viewed by others
References and Recommended Reading
Bleck TP, Greenlee JE: Subdural empyema. In Principles and Practice of Infectious Diseases, edn 5. Edited by Mandell GL, Bennett JE, Dolin R. Philadelphia: Churchill Livingstone; 2002:1028–1031. A useful, recent review that includes discussion of spinal subdural empyema. Note that this publication also includes useful reviews of intracranial and spinal epidural abscess.
Helfgott DC, Weingarten K, Hartman BJ: Subdural empyema. In Infections of the Central Nervous System, edn 2. Edited by Scheld WM, Durack DT, Whitley RJ. New York: Raven Press; 1997:495–505. An excellent, slightly older review of intracranial subdural empyema; does not discuss spinal subdural empyema. As in Bleck and Greenlee [1], this book also includes useful reviews of intracranial and spinal epidural infections.
Ariza J, Casanova A, Fernandez Viladrich F, et al.: Etiological agent and primary source of infection in 42 cases of focal intracranial suppuration. J Clin Microbiol 1986, 24:899–902.
Takoro K, Yamataki A, Nakajima F: Subdural empyema occurring 20 years after trauma: case report. Neurosurgery 1987, 21:724–726.
Kawamoto S, Nagata K, Mochizuki Y, et al.: Subdural empyema caused by hematogenous dissemination from an abscess in thigh to a preexisting chronic subdural hematoma: a case report. Neurol Med Chir Tokyo 1998, 38:743–745.
Levy I, Sood S: Staphylococcus aureus dissemination to a preexisting subdural hematoma. Pediatr Infect Dis J 2002, 15:1139–1140.
Courville CB: Subdural empyema secondary to purulent frontal sinusitis. Arch Otolaryngol 1939, 39:211–239.
Bleck TP, Greenlee JE: Approach to the patient with central nervous system infection. In Principles and Practice of Infectious Diseases, edn 5. Edited by Mandell GL, Bennett JE, Dolin R. Philadelphia: Churchill Livingstone; 2002:950–959.
Kaufman DM, Miller MH, Steigbigel NH: Subdural empyema: analysis of 17 recent cases and review of the literature. Medicine 1975, 54:485–498. Although from 1975, this article still provides an outstanding review of clinical course and symptoms.
Nathoo N, Nadvi SS, van Dellen JR, et al.: Intracranial subdural empyemas in the era of computed tomography: a review of 699 cases. Neurosurgery 1999, 44:529–535. Outstanding overview of subdural empyemas in the age of CT imaging.
Dill SR, Cobbs CG, McDonald CK: Subdural empyema: analysis of 32 cases and review. Clin Infect Dis 1995, 20:372–386.
Yoshikawa TT, Chow AW, Guze LB: Role of anaerobic bacteria in subdural empyema: report of four cases and review of 327 cases from the English literature. Am J Med 1975, 58:99–104. Although quite old, this still represents a key article in defining the major role that anaerobic organisms play in the pathogenesis of subdural empyema.
Skelton R, Maixner W, Isaacs D: Sinusitis-induced subdural empyema. Arch Dis Child 1992, 67:1478–1480.
Hutchin ME, Shores CG, Bauer MS, Yarbrough WG: Sinogenic subdural empyema and Streptococcus anginosus. Arch Otolaryngol Head Neck Surg 1999, 125:1262–1266. Good discussion of the importance of agents of the Streptococcus milleri group.
Aliaga L, Mediavilla JD, Lopez de la Osa A, et al.: Nontyphoidal salmonella intracranial infections in HIVinfected patients. Clin Infect Dise 1997, 25:1118–1120.
Komori H, Takagishi T, Otaki E, et al.: The efficacy of MR imaging in subdural empyema. Brain Dev 1992, 14:123–125.
Maytal J, Patel M, Apeatuh S, et al.: Subdural empyema in a 12-year-old girl: the value of magnetic resonance imaging. Neuroimaging 1996, 6:258–260.
de Falco R, Scarano E, Cigliano A, et al.: Surgical treatment of subdural empyema: a critical review. J Neurosurg Sci 1996, 40:53–58.
Hodges J, Anslow P, Gillett G: Subdural empyema: continuing diagnostic problems in the CT scan era. Q J Med 1986, 59:387–393.
Chen CY, Huang CC, Chang YC, et al.: Subdural empyema in 10 infants: US characteristics and clinical correlates. Radiology 1998, 207:609–617.
Tunkel AR, Wispelwey B, Scheld WM: Brain abscess. In Principles and Practice of Infectious Diseases, edn 5. Edited by Mandell GL, Bennett JE, Dolin R. Philadelphia: Churchill Livingstone; 2002:1016–1028.
Chambers HF: Penicillins. In Principles and Practice of Infectious Diseases, edn 5. Edited by Mandell GL, Bennett JE, Dolin R. Philadelphia: Churchill Livingstone; 2002:261–274.
Fekety R: Vancomycin, teicoplanin, and the streptogramins: quinuspristin and dalfopristin. In Principles and Practice of Infectious Diseases, edn 5. Edited by Mandell GL, Bennett JE, Dolin R. Philadelphia: Churchill Livingstone; 2002:382–391.
Levy RM, Gutin PH, Baskin DS, Pons VG: Vancomycin penetration of a brain abscess: case report and review of the literature. Neurosurgery 1986, 18:632–636.
Karchmer AW: Cephalosporins. In Principles and Practice of Infectious Diseases, edn 5. Edited by Mandell GL, Bennett JE, Dolin R. Philadelphia: Churchill Livingstone; 2002:174–291.
Finegold SM: Metronidazole. In Principles and Practice of Infectious Diseases, edn 5. Edited by Mandell GL, Bennett JE, Dolin R. Philadelphia: Churchill Livingstone; 2002:361–366.
Ahmed A, Loes DJ, Bressler EL: Reversible magnetic resonance imaging findings in metronidazole-induced encephalopathy. Neurology 1995, 45:588–589.
Kapoor K, Chandra M, Nag D, et al.: Evaluation of metronidazole toxicity: a prospective study. Int J Pharmacol Res 1999, 19:83–88.
Feuerman T, Wackym PA, Gade GF, et al.: Craniotomy improves outcome in subdural empyema. Surg Neurol 1989, 32:105–110.
Bok AP, Peter JC: Subdural empyema: burr holes or craniotomy? A retrospective computerized tomography-era analysis of treatment in 90 cases. J Neurosurg 1993, 78:574–578.
Kawamoto S, Nagata K, Mochizuki Y, et al.: Subdural empyema caused by hematogenous dissemination from an abscess in thigh to a preexisting chronic subdural hematoma: a case report. Neurol Med Chir Tokyo 1998, 38:743–745.
Chou CK, Chung WY, Pan HC, et al.: MRI-guided stereotactic aspiration for the treatment of deep-seated tentorial empyema: a case report. Chung Hua I Hsueh Tsa Chih Taipei 1997, 60:164–167.
Brook I: Aerobic and anaerobic bacteriology of intracranial abscesses. Pediatr Neurol 1992, 8:210–214.
Smith HP, Hendrick EB: Subdural empyema and epidural abscess in children. J Neurosurg 1983, 58:392–397.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Greenlee, J.E. Subdural Empyema. Curr Treat Options Neurol 5, 13–22 (2003). https://doi.org/10.1007/s11940-003-0019-7
Issue Date:
DOI: https://doi.org/10.1007/s11940-003-0019-7