Abstract
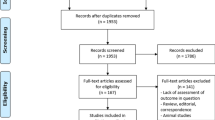
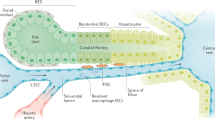
Ischaemia–reperfusion injury (IRI) in the liver, a major complication of haemorrhagic shock, resection and transplantation, is a dynamic process that involves the two interrelated phases of local ischaemic insult and inflammation-mediated reperfusion injury. This Review highlights the latest mechanistic insights into innate–adaptive immune crosstalk and cell activation cascades that lead to inflammation-mediated injury in livers stressed by ischaemia–reperfusion, discusses progress in large animal experiments and examines efforts to minimize liver IRI in patients who have received a liver transplant. The interlinked signalling pathways in multiple hepatic cell types, the IRI kinetics and positive versus negative regulatory loops at the innate–adaptive immune interface are discussed. The current gaps in our knowledge and the pathophysiology aspects of IRI in which basic and translational research is still required are stressed. An improved appreciation of cellular immune events that trigger and sustain local inflammatory responses, which are ultimately responsible for organ injury, is fundamental to developing innovative strategies for treating patients who have received a liver transplant and developed ischaemia–reperfusion inflammation and organ dysfunction.
Key Points
-
The cellular damage incurred by organ procurement and preservation affects transplantation outcomes, contributes to donor organ shortage and represents a major risk factor for acute and chronic liver graft rejection
-
Liver ischaemia–reperfusion injury (IRI) is a local proinflammatory response that is mediated by the innate immune system
-
Several pattern recognition receptors, including Toll-like receptor (TLR)4, TLR9 and the inflammasome, are involved in liver immune activation against ischaemia–reperfusion in distinct cell types at different stages of IRI development
-
Different subsets of T cells participate in innate immune responses triggered by ischaemia–reperfusion via positive and negative co-stimulatory pathways
-
Studies of regulated hepatic reperfusion in large animals might lead to successful clinical use of liver grafts procured from extended criteria donors and donation after cardiac death
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Change history
11 January 2013
In the version of this article initially published online the animal model in Figure 3 was portrayed incorrectly. The error has been corrected for the print, HTML and PDF versions of the article.
References
Wertheim, J. A., Petrowsky, H., Saab, S., Kupiec-Weglinski, J. W. & Busuttil, R. W. Major challenges limiting liver transplantation in the United States. Am. J. Transplant. 11, 1773–1784 (2011).
US Department of Health and Human Services. Organ Procurement and Transplantation Network [online], (2012).
Lentsch, A. B., Kato, A., Yoshidome, H., McMasters, K. M. & Edwards, M. J. Inflammatory mechanisms and therapeutic strategies for warm hepatic ischemia/reperfusion injury. Hepatology 32, 169–173 (2000).
Zhai, Y., Busuttil, R. W. & Kupiec-Weglinski, J. W. Liver ischemia and reperfusion injury: new insights into mechanisms of innate-adaptive immune-mediated tissue inflammation. Am. J. Transplant. 11, 1563–1569 (2011).
Eltzchig, H. K. & Eckle, T. Ischemia and reperfusion—from mechanism to translation. Nat. Med. 17, 1391–1401 (2011).
Jaeschke, H. & Woolbright, B. L. Current strategies to minimize ischemia-reperfusion injury by targeting reactive oxygen species. Transplant. Rev. 26, 103–114 (2012).
Sacks, S. H. & Zhou, W. The role of complement in the early immune response to transplantation. Nat. Rev. Immunol. 12, 431–442 (2012).
Abu-Amara, M. et al. Liver ischemia/reperfusion injury: Processes in inflammatory networks—a review. Liver Transpl. 16, 1016–1032 (2010).
Rougemont, O., Lehmann, K. & Clavien, P. A. Preconditioning, organ preservation, and postconditioning to prevent ischemia-reperfusion injury to the liver. Liver Transpl. 15, 1172–1182 (2009).
Selzner, N., Rudiger, H., Graf, R. & Clavien, P. A. Protective strategies against ischemic injury of the liver. Gastroenterology 125, 917–936 (2003).
Richards, J. A., Wigmore, S. J. & Devey, L. R. Heme oxygenase system in hepatic ischemia-reperfusion injury. World J. Gastroenterol. 16, 6068–6078 (2010).
Ikeda, T. et al. Ischemic injury in liver transplantation: difference in injury sites between warm and cold ischemia in rats. Hepatology 16, 454–461 (1992).
Shen, X. D. et al. Disruption of type-I IFN pathway ameliorates preservation damage in mouse orthotopic liver transplantation via HO-1 dependent mechanism. Am. J. Transplant. 12, 1730–1739 (2012).
Shen, X. D. et al. Inflammatory responses in a new mouse model of prolonged hepatic cold ischemia followed by arterialized orthotopic liver transplantation. Liver Transpl. 11, 1273–1281 (2005).
Land, W. et al. The beneficial effect of human recombinant superoxide dismutase on acute and chronic rejection events in recipients of cadaveric renal transplants. Transplantation 57, 211–217 (1994).
Land, W. G. The role of postischemic reperfusion injury and other nonantigen-dependent inflammatory pathways in transplantation. Transplantation 79, 505–514 (2005).
Beg, A. A. Endogenous ligands of Toll-like receptors: implications for regulating inflammatory and immune responses. Trends Immunol. 23, 509–512 (2002).
Fox-Marsh, A. & Harrison, L. C. Emerging evidence that molecules expressed by mammalian tissue grafts are recognized by the innate immune system. J. Leukoc. Biol. 71, 401–409 (2002).
Rifkin, I. R., Leadbetter, E. A., Busconi, L., Viglianti, G. & Marshak-Rothstein, A. Toll-like receptors, endogenous ligands, and systemic autoimmune disease. Immunol. Rev. 204, 27–42 (2005).
Lotze, M. T. et al. The grateful dead: damage-associated molecular pattern molecules and reduction/oxidation regulate immunity. Immunol. Rev. 220, 60–81 (2007).
Srikrishna, G. & Freeze, H. H. Endogenous damage-associated molecular pattern molecules at the crossroads of inflammation and cancer. Neoplasia 11, 615–628 (2009).
Kawai, T. & Akira, S. Toll-like receptor and RIG-I-like receptor signaling. Ann. NY Acad. Sci. 1143, 1–20 (2008).
Takeuchi, O. & Akira, S. Pattern recognition receptors and inflammation. Cell 140, 805–820 (2010).
Akira, S. & Takeda, K. Toll-like receptor signalling. Nat. Rev. Immunol. 4, 499–511 (2004).
Trinchieri, G. & Sher, A. Cooperation of Toll-like receptor signals in innate immune defence. Nat. Rev. Immunol. 7, 179–190 (2007).
Baccala, R. et al. Sensors of the innate immune system: their mode of action. Nat. Rev. Rheumatol. 5, 448–456 (2009).
Tsung, A. et al. Hepatic ischemia/reperfusion injury involves functional TLR4 signaling in nonparenchymal cells. J. Immunol. 175, 7661–7668 (2005).
Wu, H. S. et al. Toll-like receptor 4 involvement in hepatic ischemia/reperfusion injury in mice. Hepatobiliary Pancreat. Dis. Int. 3, 250–253 (2004).
Zhai, Y. et al. Cutting edge: TLR4 activation mediates liver ischemia/reperfusion inflammatory response via IFN regulatory factor 3-dependent MyD88-independent pathway. J. Immunol. 173, 7115–7119 (2004).
Leemans, J. C. et al. Renal-associated TLR2 mediates ischemia/reperfusion injury in the kidney. J. Clin. Invest. 115, 2894–2903 (2005).
Arslan, F. et al. Myocardial ischemia/reperfusion injury is mediated by leukocytic Toll-like receptor-2 and reduced by systemic administration of a novel anti-Toll-like receptor-2 antibody. Circulation 121, 80–90 (2010).
Shen, X. D. et al. Absence of toll-like receptor 4 (TLR4) signaling in the donor organ reduces ischemia and reperfusion injury in a murine liver transplantation model. Liver Transpl. 13, 1435–1443 (2007).
Ellett, J. D. et al. Toll-like receptor 4 is a key mediator of murine steatotic liver warm ischemia/reperfusion injury. Liver Transpl. 15, 1101–1109 (2009).
Hui, W., Jinxiang, Z., Heshui, W., Zhuoya, L. & Qichang, Z. Bone marrow and non-bone marrow TLR4 regulates hepatic ischemia/reperfusion injury. Biochem. Biophys. Res. Commun. 389, 328–332 (2009).
Wu, H. et al. TLR4 activation mediates kidney ischemia/reperfusion injury. J. Clin. Invest. 117, 2847–2859 (2007).
Pulskens, W. P. et al. Toll-like receptor-4 coordinates the innate immune response of the kidney to renal ischemia/reperfusion injury. PLoS ONE 3, e3596 (2008).
Kaczorowski, D. J. et al. Mechanisms of Toll-like receptor 4 (TLR4)-mediated inflammation after cold ischemia/reperfusion in the heart. Transplantation 87, 1455–1463 (2009).
Shigeoka, A. A. et al. TLR2 is constitutively expressed within the kidney and participates in ischemic renal injury through both MyD88-dependent and -independent pathways. J. Immunol. 178, 6252–6258 (2007).
Broad, A., Kirby, J. A. & Jones, D. E. Toll-like receptor interactions: tolerance of MyD88-dependent cytokines but enhancement of MyD88-independent interferon-beta production. Immunology 120, 103–111 (2007).
Biswas, S. K. & Lopez-Collazo, E. Endotoxin tolerance: new mechanisms, molecules and clinical significance. Trends Immunol. 30, 475–487 (2009).
Martin, M., Rehani, K., Jope, R. S. & Michalek, S. M. Toll-like receptor-mediated cytokine production is differentially regulated by glycogen synthase kinase 3. Nat. Immunol. 6, 777–784 (2005).
Ren, F. et al. Inhibition of glycogen synthase kinase 3 beta ameliorates liver ischemia reperfusion injury by way of an interleukin-10-mediated immune regulatory mechanism. Hepatology 54, 687–696 (2011).
Jacob, A. I., Goldberg, P. K., Bloom, N., Degenshein, G. A. & Kozinn, P. J. Endotoxin and bacteria in portal blood. Gastroenterology 72, 1268–1270 (1977).
Fiorini, R. N. et al. Anti-endotoxin monoclonal antibodies are protective against hepatic ischemia/reperfusion injury in steatotic mice. Am. J. Transplant. 4, 1567–1573 (2004).
Zhai, Y. et al. Evidence for the pivotal role of endogenous toll-like receptor 4 ligands in liver ischemia and reperfusion injury. Transplantation 85, 1016–1022 (2008).
Erridge, C. Endogenous ligands of TLR2 and TLR4: agonists or assistants? J. Leukoc. Biol. 87, 989–999 (2010).
Tsung, A. et al. The nuclear factor HMGB1 mediates hepatic injury after murine liver ischemia-reperfusion. J. Exp. Med. 201, 1135–1143 (2005).
Tsung, A. et al. HMGB1 release induced by liver ischemia involves Toll-like receptor 4 dependent reactive oxygen species production and calcium-mediated signaling. J. Exp. Med. 204, 2913–2923 (2007).
Hreggvidsdottir, H. S. et al. The alarmin HMGB1 acts in synergy with endogenous and exogenous danger signals to promote inflammation. J. Leukoc. Biol. 86, 655–662 (2009).
Qin, Y. H. et al. HMGB1 enhances the proinflammatory activity of lipopolysaccharide by promoting the phosphorylation of MAPK p38 through receptor for advanced glycation end products. J. Immunol. 183, 6244–6250 (2009).
Zeng, S. et al. Receptor for advanced glycation end product (RAGE)-dependent modulation of early growth response-1 in hepatic ischemia/reperfusion injury. J. Hepatol. 50, 929–936 (2009).
Zeng, S. et al. Blockade of receptor for advanced glycation end product (RAGE) attenuates ischemia and reperfusion injury to the liver in mice. Hepatology 39, 422–432 (2004).
Dhupar, R. et al. Interferon regulatory factor 1 mediates acetylation and release of high mobility group Box 1 from hepatocytes during murine liver ischemia-reperfusion injury. Shock 35, 293–301 (2011).
Ueki, S. et al. Critical role of interferon regulatory factor-1 in murine liver transplant ischemia reperfusion injury. Hepatology 51, 1692–1701 (2010).
Schiraldi, M. et al. HMGB1 promotes recruitment of inflammatory cells to damaged tissues by forming a complex with CXCL12 and signaling via CXCR4. J. Exp. Med. 209, 551–563 (2012).
Bamboat, Z. M. et al. Toll-like receptor 9 inhibition confers protection from liver ischemia-reperfusion injury. Hepatology 51, 621–632 (2009).
Huang, H. et al. Endogenous histones function as alarmins in sterile inflammatory liver injury through Toll-like receptor 9 in mice. Hepatology 54, 999–1008 (2011).
Cavassani, K. A. et al. TLR3 is an endogenous sensor of tissue necrosis during acute inflammatory events. J. Exp. Med. 205, 2609–2621 (2008).
McDonald, B. et al. Intravascular danger signals guide neutrophils to sites of sterile inflammation. Science 330, 362–366 (2010).
Zhu, P. et al. Gene silencing of NALP3 protects against liver ischemia-reperfusion injury in mice. Hum. Gene Ther. 22, 853–864 (2011).
Menzel, C. L. et al. Caspase-1 is hepatoprotective during trauma and hemorrhagic shock by reducing liver injury and inflammation. Mol. Med. 17, 1031–1038 (2011).
Suzuki, S., Toledo-Pereyra, L. H., Rodriguez, F. J. & Cejalvo, D. Neutrophil infiltration as an important factor in liver ischemia and reperfusion injury. Modulating effects of FK506 and cyclosporine. Transplantation 55, 1265–1272 (1993).
Zwacka, R. M. et al. CD4(+) T-lymphocytes mediate ischemia/reperfusion-induced inflammatory responses in mouse liver. J. Clin. Invest. 100, 279–289 (1997).
Rabb, H. et al. Pathophysiological role of T lymphocytes in renal ischemia-reperfusion injury in mice. Am. J. Physiol. Renal Physiol. 279, F525–F531 (2000).
Shen, X. D. et al. CD154-CD40 T-cell costimulation pathway is required in the mechanism of hepatic ischemia/reperfusion injury, and its blockade facilitates and depends on heme oxygenase-1 mediated cytoprotection. Transplantation 74, 315–319 (2002).
Burne, M. J. et al. Identification of the CD4+ T cell as a major pathogenic factor in ischemic acute renal failure. J. Clin. Invest. 108, 1283–1290 (2001).
Takada, M., Chandraker, A., Nadeau, K. C., Sayegh, M. H. & Tilney, N. L. The role of the B7 costimulatory pathway in experimental cold ischemia/reperfusion injury. J. Clin. Invest. 100, 1199–1203 (1997).
Shen, X. D. et al. Stat4 and Stat6 signaling in hepatic ischemia/reperfusion injury in mice: HO-1 dependence of Stat4 disruption-mediated cytoprotection. Hepatology 37, 296–303 (2003).
Kono, H. et al. Role of IL-17A in neutrophil recruitment and hepatic injury after warm ischemia-reperfusion mice. J. Immunol. 187, 4818–4825 (2011).
Caldwell, C. C., Tschoep, J. & Lentsch, A. B. Lymphocyte function during hepatic ischemia/reperfusion injury. J. Leukoc. Biol. 82, 457–464 (2007).
Radaeva, S., Sun, R., Pan, H. N., Hong, F. & Gao, B. Interleukin 22 (IL-22) plays a protective role in T cell-mediated murine hepatitis: IL-22 is a survival factor for hepatocytes via STAT3 activation. Hepatology 39, 1332–1342 (2004).
Kreymborg, K. et al. IL-22 is expressed by TH17 cells in an IL-23-dependent fashion, but not required for the development of autoimmune encephalomyelitis. J. Immunol. 179, 8098–8104 (2007).
Ki, S. H. et al. Interleukin-22 treatment ameliorates alcoholic liver injury in a murine model of chronic-binge ethanol feeding: role off signal transducer and activator of transcription 3. Hepatology 52, 1291–1300 (2010).
Wolk, K., Witte, E., Witte, K., Warszawska, K. & Sabat, R. Biology of interleukin-22. Semin. Immunopathol. 32, 17–31 (2010).
Chestovich, P. J. et al. Interleukin-22: implications for liver ischemia-reperfusion injury. Transplantation 93, 485–492 (2012).
Knolle, P. et al. Human Kupffer cells secrete IL-10 in response to lipopolysaccharide (LPS) challenge. J. Hepatol. 22, 226–229 (1995).
De Creus, A. et al. Low TLR4 expression by liver dendritic cells correlates with reduced capacity to activate allogeneic T cells in response to endotoxin. J. Immunol. 174, 2037–2045 (2005).
Bamboat, Z. M. et al. Conventional DCs reduce liver ischemia/reperfusion injury in mice via IL-10 secretion. J. Clin. Invest. 120, 559–569 (2010).
Kuchroo, V. K., Meyers, J. H., Umetsu, D. T. & DeKruyff, R. H. TIM family of genes in immunity and tolerance. Adv. Immunol. 91, 227–249 (2006).
Uchida, Y. et al. The emerging role of T cell immunoglobulin mucin-1 in the mechanism of liver ischemia and reperfusion injury in the mouse. Hepatology 51, 1363–1372 (2010).
Rong, S. et al. The TIM-1:TIM-4 pathway enhances renal ischemia-reperfusion injury. J. Am. Soc. Nephrol. 22, 484–495 (2011).
Uchida, Y. et al. T-cell immunoglobulin mucin-3 determines severity of liver ischemia/reperfusion injury in mice in a TLR4-dependent manner. Gastroenterology 139, 2195–2206 (2010).
Ji, H. et al. Programmed death-1/B7-H1 negative costimulation protects mouse liver against ischemia and reperfusion injury. Hepatology 52, 1380–1389 (2010).
Ueki, S. et al. Hepatic B7 Homolog 1 expression is essential for controlling cold ischemia/reperfusion injury after mouse liver transplantation. Hepatology 54, 216–228 (2011).
Shen, X. et al. CD4 T cells promote tissue inflammation via CD40 signaling without de novo activation in a murine model of liver ischemia/reperfusion injury. Hepatology 50, 1537–1546 (2009).
Lappas, C. M., Day, Y. J., Marshall, M. A., Engelhard, V. H. & Linden, J. Adenosine A2A receptor activation reduces hepatic ischemia reperfusion injury by inhibiting CD1d-dependent NKT cell activation. J. Exp. Med. 203, 2639–2648 (2006).
Arrenberg, P., Maricic, I. & Kumar, V. Sulfatide-mediated activation of type II natural killer T cells prevents hepatic ischemic reperfusion injury in mice. Gastroenterology 140, 646–655 (2011).
Beldi, G. et al. Deletion of CD39 on natural killer cells attenuates hepatic ischemia/reperfusion injury in mice. Hepatology 51, 1702–1711 (2010).
Magliocca, J. F. et al. Extracorporeal support for organ donation after cardiac death effectively expands the donor pool. J. Trauma 58, 1095–1101 (2005).
Fondevila, C. et al. Liver transplant using donors after unexpected cardiac death: novel preservation protocol and acceptance criteria. Am. J. Transplant. 7, 1849–1855 (2007).
Hong, J. C. et al. Regulated hepatic reperfusion mitigates ischemia and reperfusion injury and improves survival after prolonged liver warm ischemia: a pilot study on a novel concept of organ resuscitation in a large animal model. J. Am. Coll. Surg. 214, 505–515 (2012).
Garcia-Valdecasas, J. C. et al. Liver conditioning after cardiac arrest: the use of normothermic recirculation in an experimental animal model. Transpl. Int. 11, 424–432 (1998).
Fondevila, C. et al. Superior preservation of DCD livers with continuous normothermic perfusion. Ann. Surg. 254, 1000–1007 (2011).
Monbaliu, D. & Brassil, J. Machine perfusion of the liver: past, present and future. Curr. Opin. Organ. Transplant. 15, 160–166 (2010).
Butler, A. J. et al. Successful extracorporeal porcine liver perfusion for 72 hr. Transplantation 73, 1212–1218 (2002).
Schon, M. R. et al. Liver transplantation after organ preservation with normothermic extracorporeal perfusion. Ann. Surg. 233, 114–123 (2001).
Brockmann, J. et al. Normothermic perfusion: a new paradigm for organ preservation. Ann. Surg. 250, 1–6 (2009).
de Rougemont, O. et al. One hour hypothermic oxygenated perfusion (HOPE) protects nonviable liver allografts donated after cardiac death. Ann. Surg. 250, 674–683 (2009).
Guarrera, J. V. et al. Hypothermic machine preservation in human liver transplantation: the first clinical series. Am. J. Transplant. 10, 372–381 (2010).
Minor, T., Manekeller, S., Sioutis, M. & Dombrowski, F. Endoplasmic and vascular surface activation during organ preservation: refining upon the benefits of machine perfusion. Am. J. Transplant. 6, 1355–1366 (2006).
Goto, M. et al. Hepatic tissue oxygenation as a predictive indicator of ischemia-reperfusion liver injury. Hepatology 15, 432–437 (1992).
Kamiike, W. et al. Correlation between cellular ATP level and bile excretion in the rat liver. Transplantation 39, 50–55 (1985).
Monden, M. & Fortner, J. G. Twenty-four- and 48-hour canine liver preservation by simple hypothermia with prostacyclin. Ann. Surg. 196, 38–42 (1982).
Ghonem, N. et al. Treprostinil, a prostacyclin analog, ameliorates ischemia-reperfusion injury in rat orthotopic liver transplantation. Am. J. Transplant. 11, 2508–2516 (2011).
Klein, M. et al. Preconditioning of donor livers with prostaglandin I2 before retrieval decreases hepatocellular ischemia-reperfusion injury. Transplantation 67, 1128–1132 (1999).
Kotsch, K. et al. Methylprednisolone therapy in deceased donors reduces inflammation in the donor liver and improves outcome after liver transplantation: a prospective randomized controlled trial. Ann. Surg. 248, 1042–1050 (2008).
Weiss, S. et al. Brain death activates donor organs and is associated with a worse I/R injury after liver transplantation. Am. J. Transplant. 7, 1584–1593 (2007).
Mehrabi, A. et al. Thymoglobulin and ischemia reperfusion injury in kidney and liver transplantation. Nephrol. Dial. Transplant. 22 (Suppl. 8), viii54–viii60 (2007).
Goggins, W. C. et al. A prospective randomized clinical trial of intraoperative versus postoperative thymoglobulin in adult cadaveric renal transplant recipients. Transplantation 76, 798–802 (2003).
Bogetti, D. et al. Thymoglobulin induction protects liver allografts from ischemia/reperfusion injury. Clin. Transplant. 19, 507–511 (2005).
Baskin-Bey, E. S. et al. Clinical trial of the pan-caspase inhibitor, IDN-6556, in human liver preservation injury. Am. J. Transplant. 7, 218–225 (2007).
Alvarado-Kristensson, M. et al. p38-MAPK signals survival by phosphorylation of caspase-8 and caspase-3 in human neutrophils. J. Exp. Med. 199, 449–458 (2004).
Busuttil, R. W. et al. rPSGL-Ig for improvement of early liver allograft function: a double-blind, placebo-controlled, single-center phase II study. Am. J. Transplant. 11, 786–797 (2011).
Yang, J., Galipeau, J., Kozak, C. A., Furie, B. C. & Furie, B. Mouse P-selectin glycoprotein ligand-1: molecular cloning, chromosomal localization, and expression of a functional P-selectin receptor. Blood 87, 4176–4186 (1996).
Dulkanchainun, T. S. et al. Reduction of hepatic ischemia/reperfusion injury by a soluble P-selectin glycoprotein ligand-1. Ann. Surg. 227, 832–840 (1998).
Amersi, F. et al. P-selectin glycoprotein ligand-1 (rPSGL-Ig)-mediated blockade of CD62 selectin molecules protects rat steatotic liver grafts from ischemia/reperfusion injury. Am. J. Transplant. 2, 600–608 (2002).
Tsuchihashi, S. et al. Molecular characterization of rat leukocyte P-selectin glycoprotein ligand-1 and effect of its blockade: protection from ischemia-reperfusion injury in liver transplantation. J. Immunol. 176, 616–624 (2006).
Lang, J. D. et al. Inhaled NO accelerates restoration of liver function in adults following orthotopic liver transplantation. J. Clin. Invest. 117, 2583–2591 (2007).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2009).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
US National Library of Medicine. ClinicalTrials.gov [online], (2012).
Kristo, I. et al. Effect of intraportal infusion of tacrolimus on ischaemic reperfusion injury in orthotopic liver transplantation: a randomized controlled trial. Transpl. Int. 24, 912–919 (2011).
Khan, A. W. et al. A prospective randomized trial of N-acetyl cysteine administration during cold preservation of the donor liver for transplantation. Ann. Hepatol. 4, 121–126 (2005).
Hilmi, I. A. et al. N-acetylcysteine does not prevent hepatorenal ischaemia-reperfusion injury in patients undergoing orthotopic liver transplantation. Nephrol. Dial Transplant. 25, 2328–2333 (2010).
ISRCTN Register. HEGPOL: Randomised, placebo controlled, multicenter, double-blind clinical trial to investigate hepatoprotective effects of glycine in the postoperative phase of liver transplantation [online], (2012).
Author information
Authors and Affiliations
Contributions
All authors contributed equally to researching data for the article, discussions of content and reviewing and editing the manuscript. Y. Zhai, H. Petrowsky, J. C. Hong and J. W. Kupiec-Weglinski wrote the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Zhai, Y., Petrowsky, H., Hong, J. et al. Ischaemia–reperfusion injury in liver transplantation—from bench to bedside. Nat Rev Gastroenterol Hepatol 10, 79–89 (2013). https://doi.org/10.1038/nrgastro.2012.225
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2012.225
This article is cited by
-
Dynamic changes in the mouse hepatic lipidome following warm ischemia reperfusion injury
Scientific Reports (2024)
-
Insulin-induced gene 2 protects against hepatic ischemia–reperfusion injury via metabolic remodeling
Journal of Translational Medicine (2023)
-
VEGFR2 targeted microbubble-based ultrasound molecular imaging improving the diagnostic sensitivity of microinvasive cervical cancer
Journal of Nanobiotechnology (2023)
-
Hepatocyte SGK1 activated by hepatic ischemia-reperfusion promotes the recurrence of liver metastasis via IL-6/STAT3
Journal of Translational Medicine (2023)
-
Targeting ferroptosis by poly(acrylic) acid coated Mn3O4 nanoparticles alleviates acute liver injury
Nature Communications (2023)