Abstract
Objective: Since inordinately long or short lengths of stay at hospice can create problems for patients, providers, and payers, the author sought to identify predictors of timing of patient referral.
Methods: A retrospective cohort of 405 hospice outpatients was analyzed with Cox regression to evaluate the effect on length of stay of patient age, gender, race, diagnosis, activity level, mental status, dyspnea, insurance, income, religion, and home support, and of referring physician specialty.
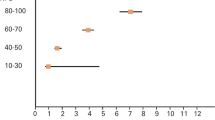
Results: Median survival time at the hospice was 29 days; 15% of the patients died within seven days and 12% lived longer than 180 days. A one-unit increment in a six-unit activity-level scale was associated with a 19% reduction in the rate of death. Compared with reference groups, oriented patients and depressed patients had 57% and 35% lower death rates; patients with prostate cancer and cardiovascular disease had 50% and 58% lower death rates. There was no significant gender, race, religion, insurance, or income difference among the patient groups.
Conclusions: Inappropriately early or late referral occurs in a substantial minority of patients referred to the hospice under study. Closer attention to accurate prognostication in different types of terminally ill patients and more timely referral to hospice might help to optimize the use of this health care resource from both patient and societal perspectives.
Similar content being viewed by others
References
Greer D, Mor V, Morris J, Sherwood S, Kidder D, Birnbaum H. An alternative in terminal care: results of the National Hospice Study. J Chron Dis. 1986;39:9–26.
Kane RI, Klein SJ, Bernstein L, Rothenberg R, Wales J. Hospice role in alleviating the emotional stress of terminal patients and their families. Med Care. 1985;23:189–97.
Dawson NJ. Need satisfaction in terminal care settings. Soc Sci Med. 1991;32:83–7.
Kidder D. The effects of hospice coverage on Medicare expenditures. Health Serv Res. 1992;27:195–217.
Mor V, Kidder D. Cost savings in hospice: final results of the National Hospice Study. Health Serv Res. 1985;20:407–21.
Bloom BS, Kissick PD. Home and hospital cost of terminal illness. Med Care. 1980;18:560–4.
Mor V, Greer DS, Kastenbaum R. The Hospice Experiment. Baltimore: Johns Hopkins Press, 1988.
Data available from the National Hospice Organization, Arlington, VA, and partially reprinted in: National Hospice Organization. 1990 hospice statistics compiled. NHO Newsline. 1991;1(10):1.
Davis FA. Medicare hospice benefit: early program experience. Health Care Financing Rev. 1988;9:99–111.
Bulkin W, Lukashok H. Rx for dying: the case for hospice. N Engl J Med. 1988;318:376–8.
Knaus WA, Wagner DP, Lynn J. Short-term mortality predictions for critically ill hospitalized adults: science and ethics. Science. 1991;254:389–94.
Detsky AS, Stricker SC, Mulley AG, Thibault GE. Prognosis, survival, and the expenditure of hospital resources for patients in an intensive care unit. N Engl J Med. 1981;305:667–72.
Perkins HS, Jonsen AR, Epstein WV. Providers as predictors: using outcome predictions in intensive care. Crit Care Med. 1986;14:105–10.
Schonwetter RS, Teasdale TA, Storey P, Luchi RJ. Estimation of survival time in terminal cancer patients: an impedance to hospice admissions? Hospice J. 1990;6:65–79.
Reuben DB, Mor V, Hiris J. Clinical symptoms and length of survival in patients with terminal cancer. Arch Intern Med. 1988;148:1586–91.
Forster LE, Lynn J. Predicting life span for applicants to inpatient hospice. Arch Intern Med. 1988;148:2540–3.
Forster LE, Lynn J. The use of physiologic measures and demographic variables to predict longevity among inpatient hospice applicants. Am J Hospice Palliat Care. 1989;6:31–4.
Infeld DL, Crum GE, Koshuta MA. Characteristics of patients in a long-term care hospice setting. Hospice J. 1990;6:81–104.
Hyman RB, Bulkin W. Physician reported incentives and disincentives for referring patients to hospice. Hospice J. 1990;6:39–64.
Pearlman RA. Inaccurate predictions of life expectancy: dilemmas and opportunities. Arch Intern Med. 1988;148:2537–8.
Brody H, Lynn J. The physician’s responsibility under the new Medicare reimbursement for hospice care. N Engl J Med. 1984;310:920–2.
Based on data from: Philadelphia Department of Public Health. Selected Resident Birth and Death Data by Health District, by Census Tract, and by Neighborhood, 1990. Philadelphia: Department of Public Health, 1991.
Kriebel M. A profile of hospice programs in Pennsylvania. Hospice J. 1989;5:51–71.
Allison PD. Event History Analysis: Regression for Longitudinal Event Data. Newbury Park, CA: Sage Publications, 1984.
Teachman JD, Hayward MD. Interpreting hazard rate models. Sociol Methods Res. 1993;21(3):340–71.
HCFA Health Policy Research Center. Medicare hospice enrollment and reimbursement analysis [draft document]. Baltimore: HCFA, 1993.
Briggs PG. Who needs a hospice? Med J Aust. 1992;156:417–20.
Peterson AV. Bounds for a joint distribution with fixed sub-distribution functions: application to competing risks. Proc. Natl Acad Sci USA. 1976;93:11–3.
Magee L. R2 measures based on Wald and likelihood ratio joint significance tests. Am Statist. 1990;44:250–3.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Statist Assoc. 1958;53:457–81.
Evans C, McCarthy M. Prognostic uncertainty in terminal care: can the Karnofsky index help? Lancet. 1985;1:1204–6.
Mor V, Lalibert L, Morris JN, Wiemann M. The Karnofsky performance status scale: an examination of its reliability and validity in a research setting. Cancer. 1984;53:2002–7.
Cassileth BR, Lusk EJ, Miller DS, Brown LL, Miller C. Psychosocial correlates of survival in advanced malignant disease? N Engl J Med. 1985;312:1551–5.
Zuckerman DM, Kasl SV, Ostfeld AM. Psychosocial predictors of mortality among the elderly poor: the role of religion, well-being, and social contacts. Am J Epidemiol. 1984;119:410–23.
Idler EL, Kasl SV. Religion, disability, depression, and the timing of death. Am J Sociol. 1992;97:1052–79.
Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction: impact on 6-month survival. JAMA. 1993;270:1819–25.
Kübler-Ross E. On Death and Dying. New York: Macmillan, 1969.
Reuben DB, Mor V. Dyspnea in terminally ill cancer patients. Chest. 1986;89:234–6.
Jarvis GK, Northcott HC. Religion and differences in morbidity and mortality. Soc Sci Med. 1987;25:813–24.
Phillips DP, Smith DG. Postponement of death until symbolically meaningful occasions. JAMA. 1990;263:1947–51.
Schoenbach VJ, Kaplan BH, Fredman L, Kleinbaum DG. Social ties and mortality in Evans County, Georgia. Am J Epidemiol. 1986;123:577–91.
HCFA Health Policy Research Center. High Cost Hospice Care: Final Report. Baltimore: HCFA, 1991.
Author information
Authors and Affiliations
Additional information
Received from the Division of General Internal Medicine, Leonard Davis Institute of Health Economics, Department of Sociology, University of Pennsylvania, Philadelphia, Pennsylvania.
Supported by the Robert Wood Johnson Foundation Clinical Scholars Program and by the Warren-Whitman-Richardson Fellowship from Harvard Medical School. Dr. Christakis is the recipient of a NRSA Fellowship from the Agency for Health Care Policy and Research. Computer facilities were provided by the Department of Sociology, University of Pennsylvania.
The opinions and conclusions herein are the author’s and do not necessarily represent the views of the Robert Wood Johnson Foundation.
Rights and permissions
About this article
Cite this article
Christakis, N.A. Timing of referral of terminally Ill patients to an outpatient hospice. J Gen Intern Med 9, 314–320 (1994). https://doi.org/10.1007/BF02599178
Issue Date:
DOI: https://doi.org/10.1007/BF02599178