Abstract
Objective
To investigate whether pathological changes in elbow epicondylopathy, as assessed by conventional ultrasonography and clinical outcomes, could be modified following tenotomy with platelet-rich plasma (PRP) versus tenotomy with lidocaine.
Methods
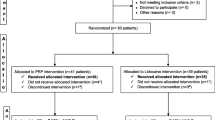
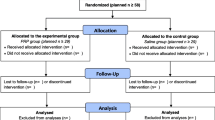
This prospective sub-study was part of a patient- and assessor-blinded, superiority-type, randomized, lidocaine-controlled trial that was performed in a tertiary hospital to assess the effectiveness of PRP versus lidocaine as tenotomy adjuvants in patients with epicondylopathy. Patients were followed after two sessions of tenotomy with either PRP or lidocaine adjuvants (4 ml) within a 2-week interval. Tendon thickness, echotexture, and neovascularization were assessed as secondary outcome measurements at baseline and at 3, 6, 12, and 20 months after treatment, and correlations with clinical outcomes were examined.
Results
Twenty months after treatment, tenotomy induced changes in tendon structure, thickness (± = 0.0006), vascularity (p < 0.0001), and echotexture (p < 0.0001). In Disabilities of the Arm, Shoulder and Hand (DASH-E) and pain (VAS-P) scores, 80.85% and 90.91% of patients showed a meaningful clinical improvement, respectively, without differences between PRP and lidocaine. There were significant differences in between-group changes in vascularity over time, p = 0.037 and p = 0.049 in the unadjusted and adjusted models, respectively. There was no relationship between pain or function and sonographic entities at the various time points.
Conclusions
Two successive needle tenotomies induced structural changes in recalcitrant epicondylopathy, with PRP displaying more vascularization and increased thickness over time compared to lidocaine. PRP compared with lidocaine did not result in improved function or decreased pain over 20 months.





Similar content being viewed by others
References
D'Addona A, Maffulli N, Formisano S, Rosa D. Inflammation in tendinopathy. Surgeon. 2017;15(5):297–302.
Andia I, Martin JI, Maffulli N. Advances with platelet-rich plasma therapies for tendon regeneration. Expert Opin Biol Ther. 2018;18(4):389–98.
Mattie R, Wong J, McCormick Z, Yu S, Saltychev M, Laimi K. Percutaneous needle tenotomy for the treatment of lateral epicondylitis: a systematic review of the literature. PM&R. 2017;9(6):603–11.
Boesen AP, Hansen R, Boesen MI, Malliaras P, Langberg H. Effect of high-volume injection, platelet-rich plasma, and sham treatment in chronic midportion Achilles tendinopathy: a randomized double-blinded prospective study. Am J Sports Med. 2017;45(9):2034–43.
Rabago D, Lee KS, Ryan M, Chourasia AO, Sesto ME, Zgierska A, et al. Hypertonic dextrose and morrhuate sodium injections (prolotherapy) for lateral epicondylosis (tennis elbow): results of a single-blind, pilot-level, randomized controlled trial. Am J Phys Med Rehabil. 2013;92(7):587–96.
Fitzpatrick J, Bulsara M, Zheng MH. The effectiveness of platelet-rich plasma in the treatment of tendinopathy: a meta-analysis of randomized controlled clinical trials. Am J Sports Med. 2017;45(1):226–33.
Miller LE, Parrish WR, Roides B, Bhattacharyya S. Efficacy of platelet-rich plasma injections for symptomatic tendinopathy: systematic review and meta-analysis of randomised injection-controlled trials. BMJ Open Sport Exerc Med. 2017;3(1):e000237.
Saltychev M, Laimi K, Virolainen P. Fredericson M. Effectiveness of platelet-rich plasma in the treatment of lateral epicondylitis-a systematic review and metaanalysis. PMR+. 2018;1(1):7–16.
Titchener AG, Booker SJ, Bhamber NS, Tambe AA, Clark DI. Corticosteroid and platelet-rich plasma injection therapy in tennis elbow (lateral epicondylalgia): a survey of current U.K. specialist practice and a call for clinical guidelines. Br J Sports Med. 2015;49(21):1410–3.
Andia I, Rubio-Azpeitia E, Maffulli N. Platelet-rich plasma modulates the secretion of inflammatory/angiogenic proteins by inflamed tenocytes. Clin Orthop Relat Res. 2015;473(5):1624–34.
Yan R, Gu Y, Ran J, et al. Intratendon delivery of leukocyte-poor platelet-rich plasma improves healing compared with leukocyte-rich platelet-rich plasma in a rabbit Achilles tendinopathy model. Am J Sports Med. 2017;45(8):1909–20.
Rubio-Azpeitia E, Bilbao AM, Sánchez P, Delgado D, Andia I. The properties of 3 different plasma formulations and their effects on tendinopathic cells. Am J Sports Med. 2016;44(8):1952–61.
Lyras D, Kazakos K, Verettas D, Polychronidis A, Simopoulos C, Botaitis S, et al. Immunohistochemical study of angiogenesis after local administration of platelet-rich plasma in a patellar tendon defect. Int Orthop. 2010;34(1):143–8.
Chaudhury S, de La Lama M, Adler RS, et al. Platelet-rich plasma for the treatment of lateral epicondylitis: sonographic assessment of tendon morphology and vascularity (pilot study). Skelet Radiol. 2013;42(1):91–7.
de Jonge S, Tol JL, Weir A, Waarsing JH, Verhaar JA, de Vos RJ. The tendon structure returns to asymptomatic values in nonoperatively treated Achilles tendinopathy but is not associated with symptoms: a prospective study. Am J Sports Med. 2015;43(12):2950–8.
Zhang YJ, Xu SZ, Gu PC, Du JY, Cai YZ, Zhang C, et al. Is platelet-rich plasma injection effective for chronic Achilles tendinopathy? A meta-analysis. Clin Orthop Relat Res. 2018;476(8):1633–41.
Dones VC 3rd, Grimmer K, Thoirs K, Suarez CG, Luker J. The diagnostic validity of musculoskeletal ultrasound in lateral epicondylalgia: a systematic review. BMC Med Imaging. 2014;14:10.
Teggeler M, Schmitz M, Fink A, Jansen JACG, Pisters MF. Reliability and agreement of ultrasonographic thickness measurements of the common lateral extensors of the elbow. Ultrasound in Med & Biol. 2015;41(6):1592–8.
Martin JI, Merino J, Atilano L, Areizaga LM, Gomez-Fernandez MC, Burgos-Alonso N, et al. Platelet-rich plasma (PRP) in chronic epicondylitis: study protocol for a randomized controlled trial. Trials. 2013;14:410.
Martin JI, Atilano L, Merino J, Gonzalez I, Iglesias G, Areizaga LM, Bully P, Grandes G, Andia I. Predictors of outcome following tenotomy in patients with recalcitrant epicondylopathy. PM&R 2018 In Press.
Martin JI, Atilano L, Merino J, Gonzalez I, Iglesias G, Areizaga LM, Bully P, Grandes G, Andia I. Platelet-rich plasma versus lidocaine as tenotomy adjuvants in people with elbow epicondylopathy: a randomized controlled trial. J Orthop Surg res. Submitted 2018.
Krogh TP, Fredberg U, Stengaard-Pedersen K, Christensen R, Jensen P, Ellingsen T. Treatment of lateral epicondylitis with platelet-rich plasma, glucocorticoid, or saline: a randomized, double-blind, placebo-controlled trial. Am J Sports Med. 2013;41(3):625–35.
Creaney L, Wallace A, Curtis M, Connell D. Growth factor-based therapies provide additional benefit beyond physical therapy in resistant elbow tendinopathy: a prospective, single-blind, randomised trial of autologous blood injections versus platelet-rich plasma injections. Br J Sports Med. 2011;45(12):966–71.
Montalvan B, Le Goux P, Klouche S, Borgel D, Hardy P, Breban M. Inefficacy of ultrasound-guided local injections of autologous conditioned plasma for recent epicondylitis: results of a double-blind placebo-controlled randomized clinical trial with one-year follow-up. Rheumatology (Oxford). 2016;55(2):279–85.
Rha DW, Park GY, Kim YK, Kim MT, Lee SC. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: a randomized controlled trial. Clin Rehabil. 2013;27(2):113–22.
Stenhouse G, Sookur P, Watson M. Do blood growth factors offer additional benefit in refractory lateral epicondylitis? A prospective, randomized pilot trial of dry needling as a stand-alone procedure versus dry needling and autologous conditioned plasma. Skelet Radiol. 2013;42(11):1515–20.
Palaniswamy V, Ng SK, Manickaraj N, et al. Relationship between ultrasound detected tendon abnormalities, and sensory and clinical characteristics in people with chronic lateral epicondylalgia. PLoS One. 2018;13(10):e0205171.
Peerbooms JC, Sluimer J, Bruijn DJ, Gosens T. Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double-blind randomized controlled trial: platelet-rich plasma versus corticosteroid injection with a 1-year follow-up. Am J Sports Med. 2010;38(2):255–62.
Acknowledgements
The authors thank Igor Gonzalez for helping in recruitment, Nuria Zuazo for monitoring data acquisition, and Mercedes Moreno and Julio del Bosque for nursing assistance.
Funding
This work was supported by “Instituto de Salud Carlos III”, ISCIII (grant number PI13/01707 to I.A.) and co-financed by FEDER funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Clinical trial registration: Ethics approval and consent to participate
This study was approved by the Ethics Committee of Hospital Universitario Cruces (No. CEIC 13/04). All enrolled patients provided written informed consent. The study protocol was registered at ClinicalTrials.gov (identifier NCT01945528) EUDRACT No.2013–000478-32.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martin, J.I., Atilano, L., Bully, P. et al. Needle tenotomy with PRP versus lidocaine in epicondylopathy: clinical and ultrasonographic outcomes over twenty months. Skeletal Radiol 48, 1399–1409 (2019). https://doi.org/10.1007/s00256-019-03193-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-019-03193-1