Abstract
Purpose
We aimed to investigate the possible factors associated with the occurrence of crossed cerebellar diaschisis (CCD) at the hyperacute stage of ischemic stroke using whole-brain volume perfusion CT (VPCT) combined with magnetic resonance imaging (MRI).
Materials and methods
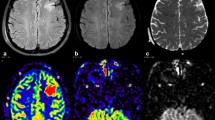
We retrospectively analyzed 108 patients with ischemic stroke within 6 h of onset. The VPCT findings of the patients showed a unilateral perfusion deficit in the supratentorial territory. Follow-up MRI examinations were performed within 24 h after onset. The effects of the supratentorial cerebral ischemia, the location distribution, the final infarct volume and the apparent diffusion coefficient (ADC) value on the occurrence and severity of CCD were analyzed.
Results
Among 108 patients with hyperacute cerebral ischemia, 62 (57.4%) demonstrated a contralateral cerebellar perfusion deficit on the VPCT maps. The occurrence of CCD was related to a reduction in cerebral blood volume (CBV) and prolongation of the mean transit time (MTT). Notably, the decrease in the ADC value in the infarct based on follow-up MRI was closely related to the occurrence and severity of CCD.
Conclusion
The occurrence and severity of CCD are related to the degree of low supratentorial perfusion and the decrease in the ADC value of infarct focus.


Similar content being viewed by others
References
Komaba Y, Mishina M, Utsumi K, Katayama Y, Kobayashi S, Mori O. Crossed cerebellar diaschisis in patients with cortical infarction: logistic regression analysis to control for confounding effects. Stroke. 2004;35:472–6.
Baron JC, Bousser MG, Comar D, Castaigne P. “Crossed cerebellar diaschisis” in human supratentorial brain infarction. Trans Am Neurol Assoc. 1981;105:459–61.
Ito H, Kanno I, Shimosegawa E, Tamura H, Okane K, Hatazawa J. Hemodynamic changes during neural deactivation in human brain: a positron emission tomography study of crossed cerebellar diaschisis. Ann Nucl Med. 2002;16:249–54.
Sagiuchi T, Ishii K, Asano Y, Aoki Y, Kikuchi K, Jinguuji K, et al. Interictal crossed cerebellar hyperperfusion on Tc-99 m ECD SPECT. Ann Nucl Med. 2001;15:369–72.
Miyazaki D, Fukushima K, Nakahara A, Kodaira M, Mochizuki K, Kaneko K, et al. Crossed cerebellar diaschisis in status epilepticus. Intern Med. 2015;55:1649–51.
Niimura K, Chugani DC, Muzik O, Chugani HT. Cerebellar reorganization following cortical injury in humans: effects of lesion size and age. Neurology. 1999;52:792–7.
Otte A, Roelcke U, von Ammon K, Hausmann O, Maguire RP, Missimer J, et al. Crossed cerebellar diaschisis and brain tumor biochemistry studied with positron emission tomography, [F-18] fluorodeoxyglucose and [C-11] methionine. J Neurol Sci. 1998;156:73–7.
Soria N, Meli F, Blumenkrantz Y, Salas E, Turjanski A. Crossed cerebellar diaschisis.study of a patient by magnetic resonance imaging and positron emission tomography. Rev Neurol. 2013;56:425–8.
Takasawa M, Watanabe M, Yamamoto S, et al. Prognostic value of subacute crossed cerebellar diaschisis: single-photon emission CT study in patients with middle cerebral artery territory infarct. Am J Neuroradiol. 2002;23:189–93.
Flint AC, Naley MC, Wright CB. Ataxic hemiparesis from strategic frontal white matter infarction with crossed cerebellar diaschisis. Stroke. 2006;37:e1–2.
Fu J, Chen WJ, Wu GY, Cheng JL, Wang MH, Zhuge Q, et al. Whole-brain 320-detector row dynamic volume CT perfusion detected crossed cerebellar diaschisis after spontaneous intracerebral hemorrhage. Neuroradiology. 2015;57:179–87.
Szilágyi G, Vas A, Kerényi L, Nagy Z, Csiba L, Gulyás B. Correlation between crossed cerebellar diaschisis and clinical neurological scales. Acta Neurol Scand. 2012;125:373–81.
Lin DD, Kleinman JT, Wityk RJ, Gottesman RF, Hillis AE, Lee AW, et al. Crossed cerebellar diaschisis in acute stroke detected by dynamic susceptibility contrast MR perfusion imaging. Am J Neuroradiol. 2009;30:710–5.
Chen S, Guan M, Lian HJ, Ma LJ, Shang JK, He S, et al. Crossed cerebellar diaschisis detected by arterial spin-labeled perfusion magnetic resonance imaging in subacute ischemic stroke. J Stroke Cerebrovasc Dis. 2014;23:2378–83.
Kang KM, Sohn CH, Kim BS, Kim YI, Choi SH, Yun TJ, et al. Correlation of asymmetry indices measured by arterial spin-labeling mr imaging and spect in patients with crossed cerebellar diaschisis. Am J Neuroradiol. 2015;36:1662–8.
Strother MK, Buckingham C, Faraco CC, Arteaga DF, Lu P, Xu Y, et al. Crossed cerebellar diaschisis after stroke identified noninvasively with cerebral blood flow-weighted arterial spin labeling MRI. Eur J Radiol. 2016;85:136–42.
Jeon YW, Kim SH, Lee JY, Whang K, Kim MS, Kim YJ, et al. Dynamic CT perfusion imaging for the detection of crossed cerebellar diaschisis in acute ischemic stroke. Korean J Radiol. 2012;13:12–9.
Biaou O, Abderahim R, Soto Ares G, Jissendi Tchofo P. Crossed cerebellar diaschisis post status epilepticus. J Radiol. 2008;89:507–9.
Ribeiro M, Beleza P, Fernandes J, Almeida F, Rocha J. Reverse crossed cerebellar diaschisis. Acta Med Port. 2006;19:439–41.
Dodick DW, Roarke MC. Crossed cerebellar diaschisis during migraine with prolonged aura: a possible mechanism for cerebellar infarctions. Cephalalgia. 2008;28:83–6.
Kunz WG, Sommer WH, Höhne C, Fabritius MP, Schuler F, Dorn F, et al. Crossed cerebellar diaschisis in acute ischemic stroke: impact on morphologic and functional outcome. J Cereb Blood Flow Metab. 2017;37:3615–24.
Sommer WH, Bollwein C, Thierfelder KM, Baumann A, Janssen H, Ertl-Wagner B, et al. Crossed cerebellar diaschisis in patients with acute middle cerebral artery infarction: occurrence and perfusion characteristics. J Cereb Blood Flow Metab. 2016;36:743–54.
Liu J, Li J, Yang Y, Wang X, Zhang Z, Zhang L. Neuronal apoptosis in cerebral ischemia/reperfusion area following electrical stimulation of fastigial nucleus. Neural Regen Res. 2014;9:727–34.
Nocuń A, Wojczal J, Szczepańska-Szerej H, Wilczyński M, Chrapko B. Quantitative evaluation of crossed cerebellar diaschisis, using voxel-based analysis of Tc-99 m ECD brain SPECT. Nucl Med Rev Cent East Eur. 2013;16:31–4.
Gharbawie OA, Whishaw IQ. Parallel stages of learning and recovery of skilled reaching after motor cortex stroke : “oppositions”organize normal and compensatory movements. Behav Brain Res. 2006;175:249–62.
Kim SE, Choi CW, Yoon BW, Chung JK, Roh JH, Lee MC, et al. Crossed-cerebellar diaschisis in cerebral infarction: technetium-99 m-HMPAO SPECT and MRI. J Nucl Med. 1997;38:14–9.
Kang KM, Sohn CH, Choi SH, Jung KH, Yoo RE, Yun TJ, et al. Detection of crossed cerebellar diaschisis in hyperacute ischemic stroke using arterial spin-labeled MR imaging. PLoS One. 2017;12:e0173971.
Kamalian S, Kamalian S, Konstas AA, Maas MB, Payabvash S, Pomerantz SR, et al. CT perfusion mean transit time maps optimally distinguish benign oligemia from true “at-risk” ischemic penumbra, but thresholds vary by postprocessing technique. Am J Neuroradiol. 2012;33:545–9.
Biesbroek JM, Niesten JM, Dankbaar JW, Biessels GJ, Velthuis BK, Reitsma JB, et al. Diagnostic accuracy of CT perfusion imaging for detecting acute ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis. 2013;35:493–501.
Shen J, Li X, Li Y, Wu B. Comparative accuracy of CT perfusion in diagnosing acute ischemic stroke: a systematic review of 27 trials. PLoS One. 2017;12:e0176622.
Sakai K, Yamada K. Machine learning studies on major brain diseases: 5-year trends of 2014–2018. Jpn J Radiol. 2019;37:34–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflicts of interest to this work.
Ethical Statement
The study was conducted with approval from our hospital review board, and the imaging data were obtained from the radiology database of our hospital. Informed consent was not required due to the retrospective nature of the study, but as a clinical routine, all patients signed the informed consent for comparative enhancement examination.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Zhang, M., Cao, Y., Wu, F. et al. Characteristics of cerebral perfusion and diffusion associated with crossed cerebellar diaschisis after acute ischemic stroke. Jpn J Radiol 38, 126–134 (2020). https://doi.org/10.1007/s11604-019-00898-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-019-00898-0