Abstract
Background
Morbidly obese (MO) patients are at increased risk for postoperative anesthesia-related complications. We evaluated the role of sugammadex versus neostigmine in the quality of recovery from profound rocuronium-induced neuromuscular blockade (NMB) in patients with morbid obesity.
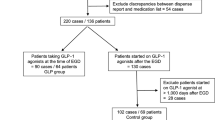
Methods
We studied 40 female MO patients who received desflurane and remifentanil anesthesia for laparoscopic removal of adjustable gastric banding. NMB was achieved with rocuronium. At the end of the surgical procedure, complete reversal of NMB was obtained with sugammadex (SUG group, n = 20) or neostigmine plus atropine (NEO group, n = 20) in the presence of profound NMB.
Results
No difference in surgical time or anesthetic drugs was found between the groups. Anesthesia time was significantly greater in the NEO group than in the SUG group (95 ± 21 vs. 47.9 ± 6.4 min, p < 0.0001), which was mainly due to a longer time to reach a train-of-four ratio (TOFR) ≥ 0.9 in the NEO group (48.6 ± 18 vs. 3.1 ± 1.3 min, p < 0.0001) during reversal of profound NMB. Upon admission to the postanesthesia care unit, level of SpO2 (p = 0.018), TOFR (p < 0.0001), ability to swallow (p = 0.0027), and ability to get into bed independently (p = 0.022) were better in the SUG group than in the NEO group. Patients in the SUG group were discharged to the surgical ward earlier than patients in the NEO group were (p = 0.013).
Conclusions
Sugammadex allowed a safer and faster recovery from profound rocuronium-induced NMB than neostigmine did in patients with MO. Sugammadex may play an important role in fast-track bariatric anesthesia


Similar content being viewed by others
References
Raeder J. Bariatric procedures as day/short stay surgery: is it possible and reasonable? Curr Opin Anaesthesiol. 2007;20(6):508–12.
Servin F. Ambulatory anesthesia for the obese patient. Curr Opin Anaesthesiol. 2006;19(6):597–9.
Murphy GS, Szokol JW, Marymont JH, et al. Residual neuromuscular blockade and critical respiratory events in the postanesthesia care unit. Anesth Analg. 2008;107(1):130–7.
Butterly A, Bittner EA, George E, et al. Postoperative residual curarization from intermediate-acting neuromuscular blocking agents delays recovery room discharge. Br J Anaesth. 2010;105(3):304–9.
Jones RK, Caldwell JE, Brull SJ, et al. Reversal of profound rocuronium-induced blockade with sugammadex: a randomized comparison with neostigmine. Anesthesiology. 2008;109(5):816–24.
Gaszynski T, Szewczyk T, Gaszynski W. Randomized comparison of sugammadex and neostigmine for reversal of rocuronium-induced muscle relaxation in morbidly obese undergoing general anaesthesia. Br J Anaesth. 2012;108(2):236–9.
Carron M, Guzzinati S, Ori C. Simplified estimation of ideal and lean body weights in morbidly obese patients. Br J Anaesth. 2012;109(5):829–30.
Bartkowski RR. Incomplete reversal of pancuronium neuromuscular blockade by neostigmine, pyridostigmine, and edrophonium. Anesth Analg. 1987;66(7):594–8.
Kopman AF. Neostigmine versus sugammadex: which, when, and how much? Anesthesiology. 2010;113(5):1010–1.
Suzuki T, Masaki G, Ogawa S. Neostigmine-induced reversal of vecuronium in normal weight, overweight and obese female patients. Br J Anaesth. 2006;97(2):160–3.
Leykin Y, Miotto L, Pellis T. Pharmacokinetic considerations in the obese. Best Pract Res Clin Anaesthesiol. 2011;25(1):27–36.
Debaene B, Plaud B, Dilly MP, et al. Residual paralysis in the PACU after a single intubating dose of nondepolarizing muscle relaxant with an intermediate duration of action. Anesthesiology. 2003;98(5):1042–8.
Carron M, Parotto E, Ori C. Prolonged neuromuscular block associated to non-alcoholic steatohepatitis in morbidly obese patient: neostigmine versus sugammadex. Minerva Anestesiol. 2012;78(1):112–3.
Vanacker BF, Vermeyen KM, Struys MM, et al. Reversal of rocuronium-induced neuromuscular block with the novel drug sugammadex is equally effective under maintenance anesthesia with propofol or sevoflurane. Anesth Analg. 2007;104(3):563–8.
Duvaldestin P, Kuizenga K, Saldien V, et al. A randomized, dose-response study of sugammadex given for the reversal of deep rocuronium- or vecuronium-induced neuromuscular blockade under sevoflurane anesthesia. Anesth Analg. 2010;110(1):74–82.
Eikermann M, Gerwig M, Hasselmann C, et al. Impaired neuromuscular transmission after recovery of the train-of-four ratio. Acta Anaesthesiol Scand. 2007;51(2):226–34.
Igarashi A, Amagasa S, Horikawa H, et al. Vecuronium directly inhibits hypoxic neurotransmission of the rat carotid body. Anesth Analg. 2002;94(1):117–22.
Eikermann M, Vogt FM, Herbstreit F, et al. The predisposition to inspiratory upper airway collapse during partial neuromuscular blockade. Am J Respir Crit Care Med. 2007;175(1):9–15.
Eriksson LI, Sundman E, Olsson R, et al. Functional assessment of the pharynx at rest and during swallowing in partially paralyzed humans: simultaneous videomanometry and mechanomyography of awake human volunteers. Anesthesiology. 1997;87(5):1035–43.
Carron M, Freo U, Ori C. Sugammadex for treatment of postoperative residual curarization in a morbidly obese patient. Can J Anaesth. 2012;59(8):813–4.
Suzuki T, Fukano N, Kitajima O, et al. Normalization of acceleromyographic train-of-four ratio by baseline value for detecting residual neuromuscular block. Br J Anaesth. 2006;96(1):44–7.
Plaud B, Debaene B, Donati F, et al. Residual paralysis after emergence from anesthesia. Anesthesiology. 2010;112(4):1013–22.
Carron M, Parotto E, Ori C. The use of sugammadex in obese patients. Can J Anaesth. 2012;59(3):321–2.
Freo U, Carron M, Innocente F, et al. Effects of A-line Autoregression Index (AAI) monitoring on recovery after sevoflurane anesthesia for bariatric surgery. Obes Surg. 2011;21(7):850–7.
Juvin P, Vadam C, Malek L, et al. Postoperative recovery after desflurane, propofol, or isoflurane anesthesia among morbidly obese patients: a prospective, randomized study. Anesth Analg. 2000;91(3):714–9.
Strum EM, Szenohradszki J, Kaufman WA, et al. Emergence and recovery characteristics of desflurane versus sevoflurane in morbidly obese adult surgical patients: a prospective, randomized study. Anesth Analg. 2004;99(6):1848–53.
La Colla L, Albertin A, La Colla G, et al. Faster wash-out and recovery for desflurane vs sevoflurane in morbidly obese patients when no premedication is used. Br J Anaesth. 2007;99(3):353–8.
McKay RE, Malhotra A, Cakmakkaya OS, et al. Effect of increased body mass index and anaesthetic duration on recovery of protective airway reflexes after sevoflurane vs desflurane. Br J Anaesth. 2010;104(2):175–82.
Bailey JM. Context-sensitive half-times and other decrement times of inhaled anesthetics. Anesth Analg. 1997;85(3):681–6.
Paul M, Fokt RM, Kindler CH, et al. Characterization of the interactions between volatile anesthetics and neuromuscular blockers at the muscle nicotinic acetylcholine receptor. Anesth Analg. 2002;95(2):362–7.
Douglas WW, Kehlet H. Management of patients in fast track surgery. BMJ. 2001;322(7284):473–6.
Chung SA, Yuan H, Chung F. A systemic review of obstructive sleep apnea and its implications for anesthesiologists. Anesth Analg. 2008;107(5):1543–63.
Gan TJ, Meyer T, Apfel CC, et al. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003;97(1):62–71.
Paraskeva A, Papilas K, Fassoulaki A, et al. Physostigmine does not antagonize sevoflurane anesthesia assessed by bispectral index or enhances recovery. Anesth Analg. 2002;94(3):569–72.
Løvstad RZ, Thagaard KS, Berner NS, et al. Neostigmine 50 microg kg(−1) with glycopyrrolate increases postoperative nausea in women after laparoscopic gynaecological surgery. Acta Anaesthesiol Scand. 2001;45(4):495–500.
Grant Information
The authors are supported by departmental funds only.
Implication
Findings from this study were presented as a poster at the 2012 International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) in New Delhi, India [Obes Surg 2012; 22: 1315-1419 (P034)].
Conflict of Interest
Michele Carron has received a payment for lecture from MSD; Mirto Foletto has received a payment for consultancy from Johnson & Johnson Medical; Carlo Ori has received payments and travel fundings for lectures and as a member of MSD Advisory Board.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carron, M., Veronese, S., Foletto, M. et al. Sugammadex Allows Fast-Track Bariatric Surgery. OBES SURG 23, 1558–1563 (2013). https://doi.org/10.1007/s11695-013-0926-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-013-0926-y